2017 EXTRA Improvement Projects
British Columbia (BC) Cancer Agency / Fraser Health (British Columbia)
- Tammy Currie, Senior Director, Regional Clinical Operations Abbotsford Centre, BC Cancer Agency, Abbotsford, British Columbia
- Marie Hawkins, Executive Director / Primary Health Care, Chronic Disease Management and Medicine Clinical Network, Fraser Health Authority, Surry, British Columbia
- Shallen Letwin, Vice President / Regional Operations, BC Cancer Agency, Vancouver, British Columbia
- Gary Pansegrau, Regional Medical Director, Fraser Valley Centre, BC Cancer Agency, Surrey, British Columbia
- Astra Pereira, Coordinator/ Regional Operations, BC Cancer Agency, Vancouver, British Columbia
Enhancing the Community Oncology Network in British Columbia
The BC Cancer Agency has oversight for the service delivery of systemic therapy, is responsible for funding all cancer drugs and for leading the development, implementation and evaluation of systemic therapy related quality standards across BC. Currently, systemic therapy (i.e. chemotherapy) is provided by both the BC Cancer Agency and the regional health authorities in BC. At the BC Cancer Agency, systemic therapy is provided across 6 regional BC Cancer Centres and within the 5 regional health authorities, systemic therapy is provided across 43 pharmacies and clinics as part of the Community Oncology Network (CON). The CON administers approximately 40% to 50% of chemotherapy within BC.
In a CON environmental scan conducted in 2016, issues were identified related to sustainability, effective care delivery, resources, quality and coordination of cancer care between organizations. By moving to an evidence-based decision making model to help inform the CON planning, decision making and operations, the IP will be tasked with the creation of provincial CON Levels of Service and CON Performance Metrics. This will improve the quality of the patient experience, help measure and monitor performance, allow for a comparison to other organizations and ensure operational excellence.
This IP is well aligned with the BC Cancer Agency, Ministry of Health and all health authority strategic priorities. It will serve to increase accountability for all providers and health care systems, while ensuring the services that support the cancer care continuum operate like an integrated system versus a fragmentation of service providers.
Centre intégré de santé et de services sociaux (CISSS) de Chaudière-Appalaches (Québec)
- Carole Bordes, Directrice adjointe Logistique, CISSS de Chaudière-Appalaches, Lévis, Québec
- Véronique Boutier, Directrice administrative de la recherche, CISSS de Chaudière-Appalaches, Lévis, Québec
- Josée Chouinard, Directrice du programme soutien à l’autonomie des personnes âgées, CISSS de Chaudière-Appalaches, Montmagny, Québec
- Daniel Paré, Président Directeur Général, CISSS de Chaudière-Appalaches, Sainte-Marie, Québec
The Care Attendant: FOR the user THROUGH Logistics
The CISSS de Chaudière-Appalaches must innovate to enhance the well-being of its population while providing good value for money. The increasing burden of cognitive disorders in long-term care facilities (CHSLDs) poses a challenge for our organization, which requires a refresh to offer a quality client experience. In this respect, the shortage of healthcare staff is a major issue.
Our project aims to maximize the tasks performed by care attendants so that they may play a pivotal role in the services provided to patients. Our working assumption is that by upgrading care attendants’ skills through a logistical analysis to pool and synchronize all work flow tasks affecting patients, care attendants will be empowered to play a privileged role in caring for patients and ensuring their well-being. These tasks should be sufficiently optimized to permit their integration without any additional cost to the organization. Beyond service optimization and greater job satisfaction for care attendants, we also expect clinical benefits for patients such as an increase in the use of non-pharmacological approaches and a decline in disruptive behaviors thanks to the presence of the care attendants.
In order to test our assumptions, we propose to carry out a comprehensive scan of planned and unplanned activities for patients in two CHSLDs in our catchment area, and to asses our interventions afterward. From an organizational standpoint, the benefits of this project will foster excellence within our institutions.
Centre intégré de santé et de services sociaux (CISSS) de la Montérégie-Centre (Québec)
- Danièle Moore, Coordonnatrice Maladies infectieuses, gestion des menaces et santé environnementale, CISSS de la Montérégie-Centre, Longueuil, Québec
- François Pilote, Professionnel équipe planification-Évaluation, Direction de santé publique, CISSS de la Montérégie-Centre, Longueuil, Québec
- Mathieu Lanthier-Veilleux, Médecin-conseil – équipe de planification et d’évaluation, CISSS de la Montérégie-Centre, Longueuil, Québec
Public Health Piloting Room: Enhanced Performance to Improve Population Health
Following the significant restructuring of Quebec’s healthcare system in 2015, every institution in the healthcare network (CISSS) set up a strategic piloting room. This proven performance management tool is used by their steering committees. Piloting rooms are used to coordinate initiatives derived from strategic plans including targets, transformative projects and completed activities.
The overarching goal of this IP is to adapt and implement a piloting room at the Direction de santé publique (DSP) de la Montérégie (Montérégie’s public health directorate), which would serve all three of its CISSS. Through its regional responsibilities, its concern with fostering staff and management engagement, as well as the challenge posed by the identification of indicators that adequately measure public health initiatives, the Directorate is looking to create a unique and adapted piloting room : democratized and multi-institutional with innovative indicators. Accordingly, through design and inclusive use (multiple professionals, orientations, stakeholders and institutions), this IP will democratize and engage resources around common priorities.
By participating in the IP’s development, the three CISSS will ensure public health related activities in our region are more consistent. Thanks to indicators that will measure public health related activities, the DSP will be in a better position to coordinate its activities and better inform other directorates with respect to their own activities, which will benefit our population’s health. Finally, the evaluation and the experimentation of this IP should inspire other directorates and other institutions to follow suit and adopt an innovative management tool.
Centre intégré de santé et de services sociaux (CISSS) de la Montérégie-Est (Québec)
- Marianne Dion-Labrie, Conseillère cadre Expérience client et Éthique, CISSS de la Montérégie-Est, Saint-Hyacinthe, Québec
- Bernard Lachance, Conseiller cadre intérimaire à la gestion intégrée de qualité, CISSS de la Montérégie-Est, Saint-Hyacinthe, Québec
- Annie Lemoine, Directrice adjointe de la qualité, de l’évaluation et de l’éthique, CISSS de la Montérégie-Est, Saint-Hyacinthe, Québec
- Michèle Ouellet, Chef à la gestion intégrée de la qualité, CISSS de la Montérégie-Est, Saint-Hyacinthe, Québec
Involving Patient Advisors in Serious Adverse Events Reviews
Risk management translates into a corrective approach aimed at reducing the consequences of an adverse event and identifying improvement measures (CISSSME, 2017). For the past few years, new approaches have been developed to foster patient and family engagement. They are directly related to the concept of "patient and family centered care" and an improved client experience. Improving Client Experience is a "set of perceptions, interactions and facts experienced by clients and families” (Beryl Institute, 2015). Patient engagement improves the quality and safety of care (Sage, 2002). Although some data points to the benefits of greater patent and family involvement, few studies confirm their actual involvement in the analysis of a serious adverse event.
This project was designed to foster the involvement of patients in reviewing these events, their voice then becoming a powerful lever for improvement. Although some patients may feel comfortable being part of such an initiative, a poorly supported and hasty involvement could lead to negative experiences. To avoid this type of outcome, the appointment of a person to support patients should lead to improved experiences. This is why patient and family support by a team of patient advisors is recommended. This project will enable the development of strategies for patient and family engagement in improvement work. It will provide the opportunity to focus on their needs, improve communication and relationships and prevent serious adverse events.
Centre intégré de santé et de services sociaux (CISSS) de la Montérégie-Ouest (Québec)
- Stéphane Dubuc, Directeur des services multidisciplinaire et de l’enseignement universitaire, CISSS de la Montérégie-Ouest, Châteauguay, Québec
- Mélanie Caron, Chef du département de pharmacie, CISSS de la Montérégie-Ouest, Châteauguay, Québec
- Sophie Poirier, Directrice adjointe, Direction des services multidisciplinaires, CISSS de la Montérégie-Ouest, Châteauguay, Québec
- Marie-Josée Roy, Directrice adjointe ID-ASD-PD(DI-TSA-DP), CISSS de la Montérégie-Ouest, Châteauguay, Québec
Innovating to Establish Community Care and Services for Stroke Patients
The healthcare reform initiated under Bill 10 requires that organizations meet a series of objectives in order to comply with the Ministry of Health and Social Services (MSSS)’s strategic plan. Among these is the implementation of a local care continuum for people who are at risk of or have suffered a stroke. An environmental scan enabled us to identify various challenges currently experienced by stroke patients such as access to care, continuity of care, especially at transition points, flow of information between different stakeholders and coordination of services.
In our current organizational structure, implementing a local continuum would depend upon the coordination of work between six clinical directorates to achieve specific time-sensitive targets. The fact that clients are spread across the entire catchment area is an additional challenge for implementing state-of-the-art practices across the continuum. Therefore, the creation of an integrated management structure for all stroke-patient related activities under a single clinical management entity appears to be an innovative solution to this sizable challenge. This project reflects our organization’s desire to focus on achieving the MSSS’s strategic priorities, the expectations of the Steering Committee regarding organizational capacity and the willingness of the Board of Directors to promote a patient as partner approach for all large-scale projects.
Centre intégré universitaire de santé et de services sociaux (CIUSSS) du Centre-Sud-de-l'île-de-Montréal (Québec)
- Donald Haineault, Directeur des soins infirmiers, CIUSSS du Centre-Sud- l'île-de-Montréal, Montréal, Québec
- Julie Grenier, Directrice adjointe au PDGA/Partenariat et soutien à l’offre de service, CIUSSS du Centre-Sud- l'île-de-Montréal, Montréal, Québec
- Julie Lajeunesse, Directrice des services professionnels, CIUSSS du Centre-Sud- l'île-de-Montréal, Montréal, Québec
- Nicole Parent, Adjointe au Directeur des soins infirmiers et directrice du projet, CIUSSS du Centre-Sud- l'île-de-Montréal, Montréal, Québec
PATH-C HND: Improvement Project - The Transition Between Hospital Care and Community Care at Notre-Dame Hospital
The integration of the Notre-Dame Hospital (HND) within the Centre intégré universitaire de santé et de services sociaux du Centre-Sud-de-l’Île-de-Montréal requires the transformation of its current vocation. The HND will change from a teaching hospital that provides subspecialty care to a community hospital that provides community care to the catchment area. A new service offering will be put together for Montreal’s downtown population to address urban healthcare issues. Population data point to poor health outcomes, mental health issues, vulnerable clients, social inequalities, and a poor fit between the population’s needs and the actual care provided.
The Improvement Project to enhance the Transition between Hospital Care and Community Care (PATH-C HND) aims to: 1) Plan a service offering in order for the HND community hospital to meet the needs of its population, including vulnerable patients who live in the city’s core, through strong local front-line care; 2) develop an optimal transition between hospital care and community care and prevent the use of emergency services through an integrated approach that promotes access, continuity and flow across the entire care journey. Based on the analysis of population’s characteristics and available evidence, the PATH-C HND project aims to define a new service offering and establish the connections required with the community to better meet the needs of downtown Montreal’s population.
Centre intégré universitaire de santé et de services sociaux (CIUSSS) du Saguenay-Lac-St-Jean (Québec)
- Céline Benoit, Directrice adjointe des services professionnels responsable de la cancérologie et des soins palliatifs, CIUSSS du Saguenay-Lac-Saint-Jean, Dolbeau-Mistassini, Québec
- Danielle Delisle, Adjointe du directeur du programme jeunesse, CIUSSS du Saguenay-Lac-Saint-Jean, Chicoutimi, Québec
- Martyne Gagnon, Conseillère-cadre services psychosociaux, CIUSSS du Saguenay-Lac-Saint-Jean, Jonquière, Québec
- Jimmy Martel, Chef de l’administration des programme équipe spécialisée en santé mentale et dépendance et services ambulatoires jeunesse, CIUSSS du Saguenay-Lac-Saint-Jean, Dolbeau-Mistassini, Québec
Quality, Accessibility and Proximity of Pediatric Palliative Care Services and Practices
From the outset, it is relevant to mention that 65% of the population served by the CIUSSS du Saguenay-Lac-Saint-Jean lives in a rural area and that our extensive catchment area is spread across 95,900 square kilometers. Quebec’s 2006 standards for pediatric palliative care define 6 categories for deaths among children: children whose condition is appropriate for a curative treatment, the outcome of which is uncertain; children whose condition will inevitably result in their premature death; children with a progressive condition with no hope of recovery; children with severe neurological problems; new-born babies whose life expectancy is very limited and family members who have unexpectedly lost a child.
In Quebec, between 1997 and 2001, the average number of annual deaths for all 6 of these categories was 840 (pediatric palliative care standards, 2006, p. 20). If one considers that Saguenay-Lac- Saint-Jean represents 3 per cent of Quebec’s total population, this translates into an average of 20 children per year on a regional basis. A quick review of 2015-16 shows 2 deaths at home, 4 deaths in hospital for non-traumatic causes and 7 youth who sought follow-up palliative care within the health and social services network. This suggests that part of our clientele dies and receives services outside of our region, information that we were unable to validate. Therefore, with a view to offer quality local care based on best practices and to meet standards established by the ministry (MSSS) in pediatric palliative care, we intend on creating a model for the organization of care and services that ensures both quality and proximity for pediatric palliative care clients despite low case volumes. In fact, most palliative care models recommend community involvement, in a broad sense, for this type of care (Plan de développement 2015-20 soins palliatifs et de fin de vie, MSSS, Québec, 2015). This aspect could be included in potential solutions to consider.
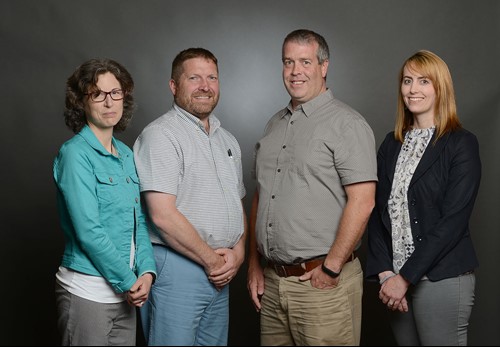
Nova Scotia Health Authority (Nova Scotia)
- Susan Stevens, Senior Director, Continuing Care, Nova Scotia Health Authority, Halifax, Nova Scotia
- Glenda Keenan, Director, System Performance, Continuing Care, Nova Scotia Health Authority, Halifax, Nova Scotia
- Scott McCulloch, Physiotherapist, Team Leader, Nova Scotia Health Authority – Senior LINCS Program, Middleton, Nova Scotia
- Bob Jenkins, Director, Continuing Care, Nova Scotia Health Authority, Yarmouth, Nova Scotia
There is No Place Like Home: Building a Home First Philosophy in the Nova Scotia Health Authority and Beyond
Since 2003/04, Nova Scotia’s health care system has experienced an important shift with more patients in hospital being discharged home with home care and fewer patients being discharged to nursing homes. Over the last several years, NSHA has seen some success in advancing the home first approach in parts of the province, however, further work is needed to develop and support a comprehensive home first culture provincially, and in particular, attention needs to be directed to those areas which haven’t achieved change.
This project will thoroughly investigate the root causes of barriers to implementing a home first culture among continuing care staff, nursing home and home care providers, acute care, primary care and mental health colleagues, physicians and individuals and families receiving continuing care. This project will also investigate the successes that have occurred in specific areas of the province to better understand best practices and critical ingredients that can be spread in other areas who have not had success. Using key performance indicators, interRAI HC data, client narratives and experiences, lessons learned from across the province and best practice literature, we will develop a Home First culture and approach. This approach will result in targeted work in specific areas to realize not only improvement to the quality of care and quality of life dimensions for individuals and families, but important health system outcomes including health care resource optimization and sustainable stewardship.
Ottawa Regional Cancer Foundation (Ontario)
- Linda Eagen, CEO, Ottawa Regional Cancer Foundation, Ottawa, Ontario
- Johanne Levesque, Senior VP Survivorship Care, Professional Practice, People and Culture, Ottawa Regional Cancer Foundation, Ottawa, Ontario
- John Ouellette, Executive VP, Ottawa Regional Cancer Foundation, Ottawa, Ontario
Improving and Spreading Cancer Coaching
Cancer Coaching is a person-centered community service developed by the Cancer Foundation in 2011. This innovative health and social care practice actively engages clients in their care to improve their quality of life and overall wellbeing. Cancer Coaching is the synthesis of global best practices. It draws from patient navigation models put forth by the Canadian Partnership Against Cancer; survivorship care (i.e., post-treatment care) from the US-based Livestrong Foundation; and, the person-centered care model designed by the UK’s MacMillan Cancer Support. It is also based on broader evidence from health coaching practices which have been shown to outperform other advice-giving approaches in 80% of clinical trials.
The Foundation has adopted the HealthChange® Methodology (Australia) which has demonstrated the value of coaching in terms of adherence to treatment plans and behavioral change when implemented across a health system. With increasing evidence of its effectiveness, the Cancer Foundation is interested in scaling up Cancer Coaching. To that end a professional training program has been developed in collaboration with York University and a community of practice has been established. Health care providers at the Winchester District Memorial Hospital, Hospice Care Ottawa, the Vanier Community Resource Center and the Rockland Family Health Team are now offering Cancer Coaching and, virtual Coaching will soon be available. The spread of Cancer Coaching will support the integration of care closer-to-home.